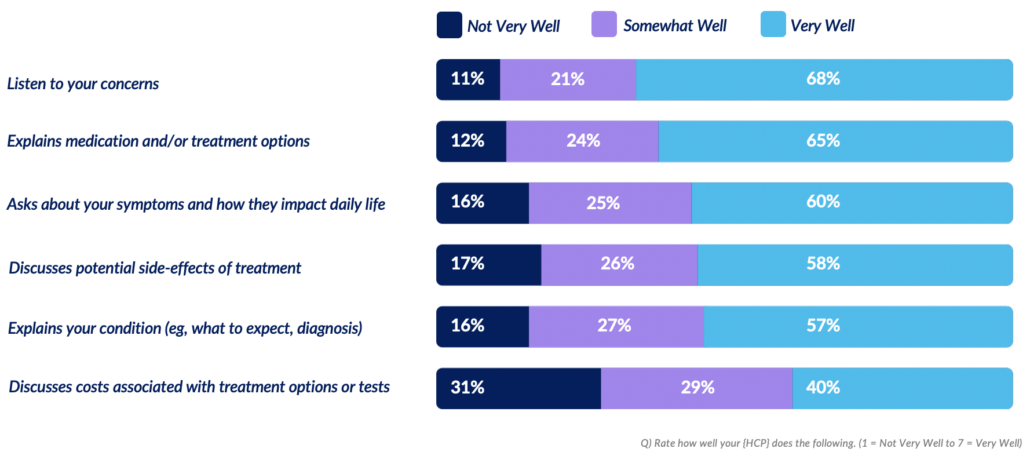
While the responses to this question provide a basic understanding of satisfaction in HCP-patient interactions, there are many aspects to the relationship not addressed.
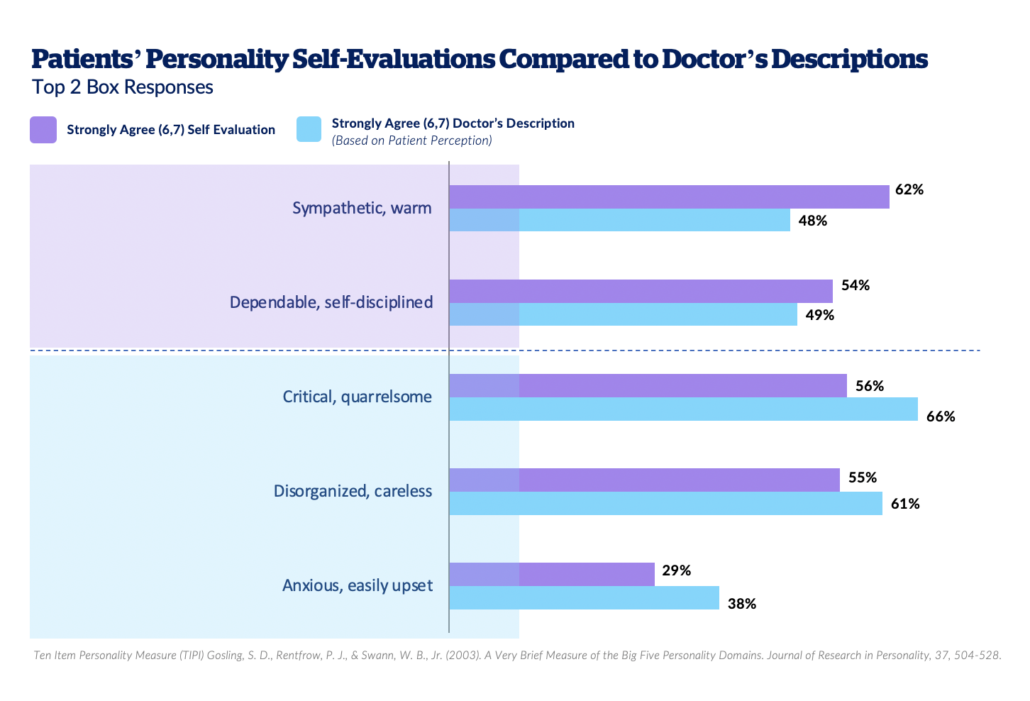
In a recent Person Before Patient survey, Health Union researchers took the opportunity to ask members of 40+ condition-specific online health communities questions that go beyond those typically asked in pharma research – focusing on topics from religion and life values to personality and pets – to better understand who they are as people, not just patients. In one section of this survey, respondents were asked to describe themselves on different personality measures, then subsequently asked to report on how they think their primary HCP views them. The responses were striking:
Patients see themselves as more sympathetic, warm, dependable, and self-disciplined than they believe their doctor does. Conversely, they feel like their doctors see them as more critical or disorganized, anxious, or easily upset than they believe they actually are. These beliefs are likely to shape how people show up to and interact with their HCP. Imagine how likely you’d be to push back on a recommendation if you believed your doctor viewed you as critical; or how likely you’d be to admit that it’s difficult to take your medication as prescribed if you believed your doctor viewed you as disorganized.
To add a qualitative, lived experience in discussing HCP-patient relationships, Health Union spoke with multiple sclerosis patient leader Dawn Morgan who shared the importance of clear, open, two-way communication between the HCP and patient to achieve the best health outcome:
“Quite often, we are as patients, we’re entering your office and we’re entering your appointment with all types of thoughts in our mind about being afraid, or will this treatment work, or how will I get my point across? How can I get my physician to understand what I’m feeling and what I’m facing? Is there an opportunity for me to really express myself? If there isn’t a line of communication from the beginning, if you aren’t able to openly and freely express yourself to your doctor, then we run into some roadblocks.”
Dawn recalled an instance when her trusted, long-time MS specialist was away on leave and she had to see a different neurologist for an appointment to discuss treatment options. “I was used to my specialist speaking with me about the health outcomes that I would like to look forward to and I felt as if she customized my treatment plan.” However, with the stand-in neurologist, Dawn “didn’t feel as if my voice was heard. I felt as if I were a child sitting on a bench and being belittled in a sense, and I just don’t find that to be the most effective way to communicate with a patient when you are in an appointment.”
She went on to add, “I did not have the greatest experience because I felt as if I were battling my doctor and I don’t feel that patients want to go into an appointment battling their healthcare provider. They looked to them for a safety net. They looked to them to be that voice that will guide them and support them. And if I were to think back long and hard, I can honestly say I did not feel supported in that particular appointment. And that is crucial.”
When asked about her ideal HCP relationship, Dawn shared that she wants both doctor and patient to walk into the appointment thinking “we are going to come together to a common goal, which is finding a treatment plan that works best for me. And that starts with getting to know who I am.” She adds, “include me in decision making, and after you’ve included me in this decision-making, allow me that time to process the information process and then discuss it with you or discuss it with someone who I trust and love at home. Sometimes decisions made on treatment plans are not just for the patient, they involve the entire family and so the relationship with the healthcare provider expands quite a bit in my opinion.”
Incorporating the Whole Person in Research
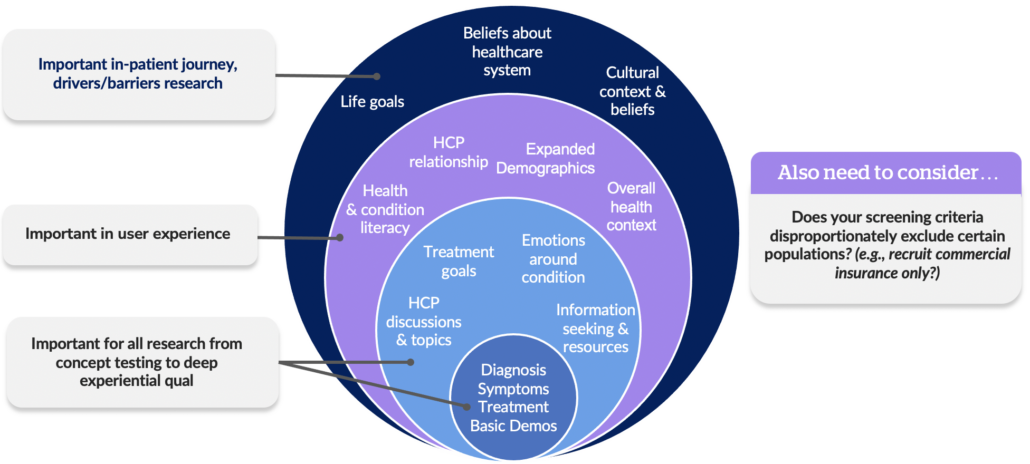
In an ideal world, aspects of the whole person would be incorporated throughout all research to better understand healthcare decision-making:
But when digging into patient journey research to really understand drivers and barriers, Health Union especially encourages you to take the time to understand who a person is outside of just their health context. Another often overlooked factor to consider in understanding the whole person is evaluating screening criteria. Some research may be intentionally or unintentionally excluding certain populations in disproportionate ways, which in turn can hinder overall understanding of the patient experience.
Understanding the whole person and how their HCP interactions impact health decisions is complex, and there’s no one-size fits all approach to uncovering these insights. However, Health Union Insights makes the following recommendations:
- In research, look for ways to incorporate time and opportunity for patients to reflect on aspects of the experience that might not be top-of-mind (or easily shareable) in a live conversation.
- Consider ways in which patient self-reported data can be used as a communication (or research) tool to help HCPs be more aware of broader patient context and considerations for care.
- Ask: How do life experiences and identities (e.g.,parental status, sexual orientation, patient experiences, professional experiences) intersect with and influence care?
Health Union Insights can help you better incorporate and understand the whole person in research, delivering smarter insights and implications, so you can spend your time developing the strategies that will make a measurable impact. Explore our Insights offerings to find out how our services can benefit your brand.