Cancer as a Chronic Condition
Beyond diagnosis and treatment, cancer has an ongoing impact on quality of life. When asked about emotions experienced since diagnosis, 75% experienced anxiety, 66% said they missed their pre-diagnosis life, 66% experienced stress and 59% said they missed their former self. Note that at the time surveyed 39% of respondents were in remission (¼ had been so for less than six months), indicating that in some cases these emotions may remain even after treatment is complete.
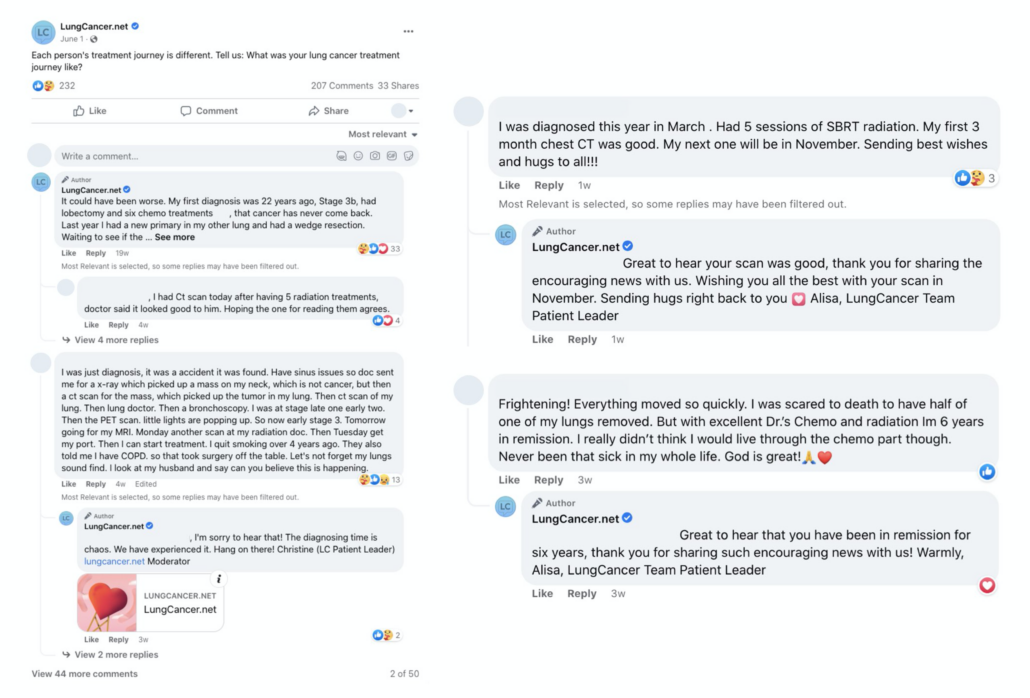
Scanxiety is a unique feeling to people living with cancer that is often discussed in social health conversations throughout oncology-related communities. According to blood cancer patient leader Amber Lynch, this feeling doesn’t end at no evidence of disease: “Survivorship after remission feels like a battle won yet the blood tests and scans can feel like a dark cloud looming. There is this constant quiet fear and building anxiety as the next scan approaches.”
Another aspect of quality of life with ongoing impact that may often be overlooked in a healthcare setting is sex and intimacy; 40%* of survey respondents indicated their desire for intimacy has been negatively impacted by cancer. Patients were prompted to share how their cancer has impacted their sex and intimacy in a short answer format and responses varied across the spectrum, which further demonstrates the uniqueness of each person’s experience:
- Prostate cancer: impacted a lot, no longer get erection/ED, can no longer ejaculate, eliminate sex drive, on Lupron, have no sex life anymore (n=159).
- Bladder cancer: bad, destroyed it, painful due to shortening of vagina, didn’t have a sex life, no impact at all (n=85).
- Advanced breast cancer: completely gone, destroyed it, no libido, affects appearance/body image, symptoms prohibit it (pain, vaginal dryness, etc.), has not affected it (n=222).
- Lung cancer: not sexually active before diagnosis, n/a, widowed, negatively, not at all (n=80).
- Blood cancer: no impact, killed all intimacy (n=11).
- Other cancers: impacted a lot, ED, no effect, symptoms prevent it (pain), no libido/interest (n=177).
Within Health Union’s oncology-focused communities, patient leaders share their experiences with sex and intimacy to spark social health conversations and help others feel less alone. In his article “Let’s Talk About Sex,” bladder cancer patient leader Jim Van Horne shares his thoughts and encouragement on the matter, while lung cancer patient leader Donna Fernandez addresses the importance of discussing intimacy with your doctor in “S-E-X and Cancer.”
The Role of Social Health
The findings from Health Union’s Beyond the Cancer Diagnosis survey combined with our immersion in social health across seven oncology-specific communities demonstrates the ongoing impact of the disease, and the importance of recognizing and treating cancer as a chronic condition. Whether newly diagnosed, currently treating or in remission, people living with cancer are engaging in social health to connect in their shared experiences – and it’s important for pharma to be meeting patients where they are.
To learn how your brand can plug into the power of social health – from scalable online health communities and social extensions to comprehensive quantitative condition-specific data and more – visit our Business Solutions page.
*Top 2 box on a 7 point scale