Challenges and Barriers are Situational
Address Challenges and Barriers Throughout the Patient Journey
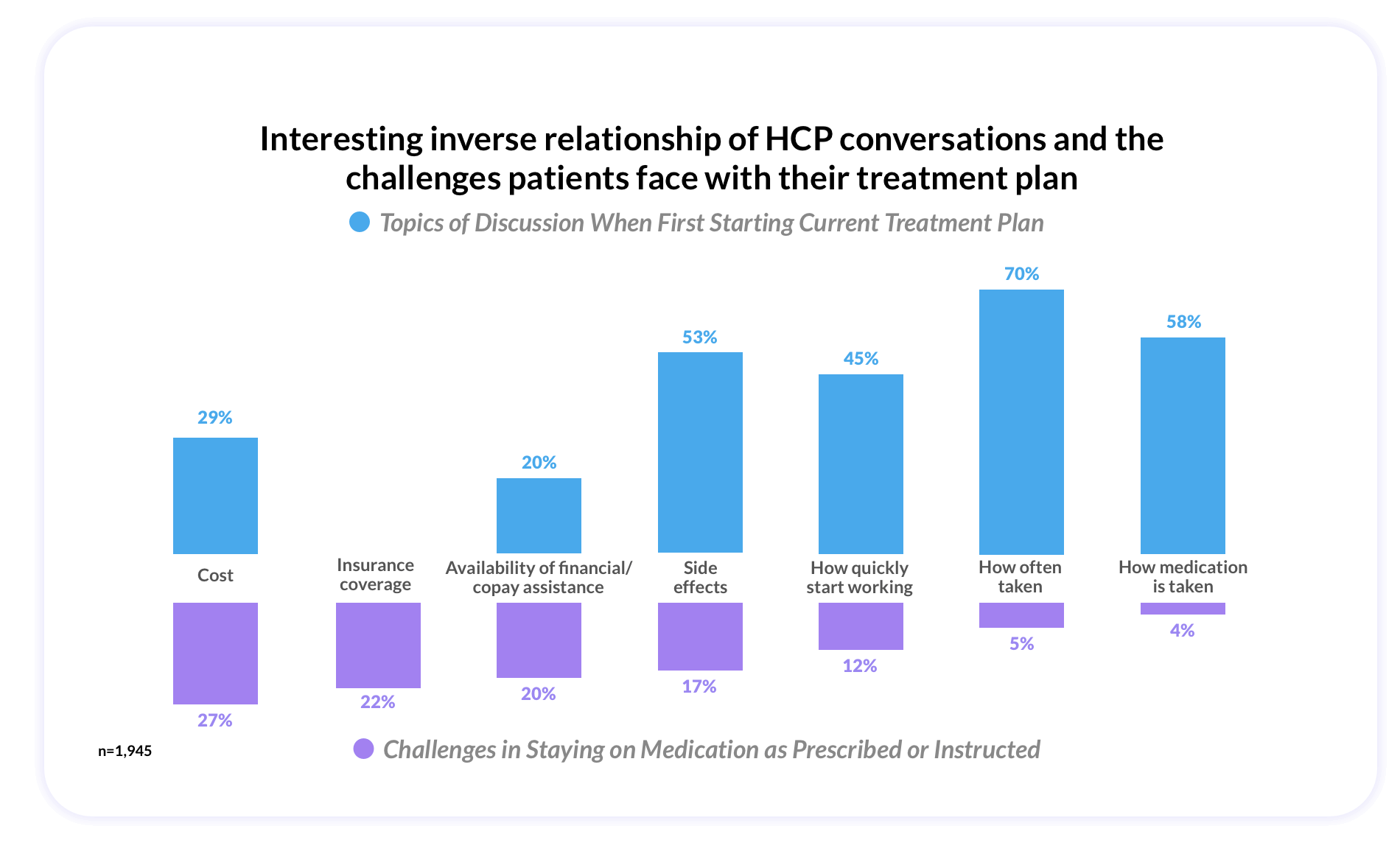
It would be simple if there were one blanket reason for these challenges and barriers, but the reality is that the reasons for nonadherence and noncompliance are situational, and thus there is not a one size fits all solution. However, we can glean insights around the critical points along a patients’ journey where nonadherence and noncompliance might come into play.
Our research identified some themes based on points within the patient journey, which may help healthcare providers, payers, and pharmaceutical companies understand where the barriers may lie.
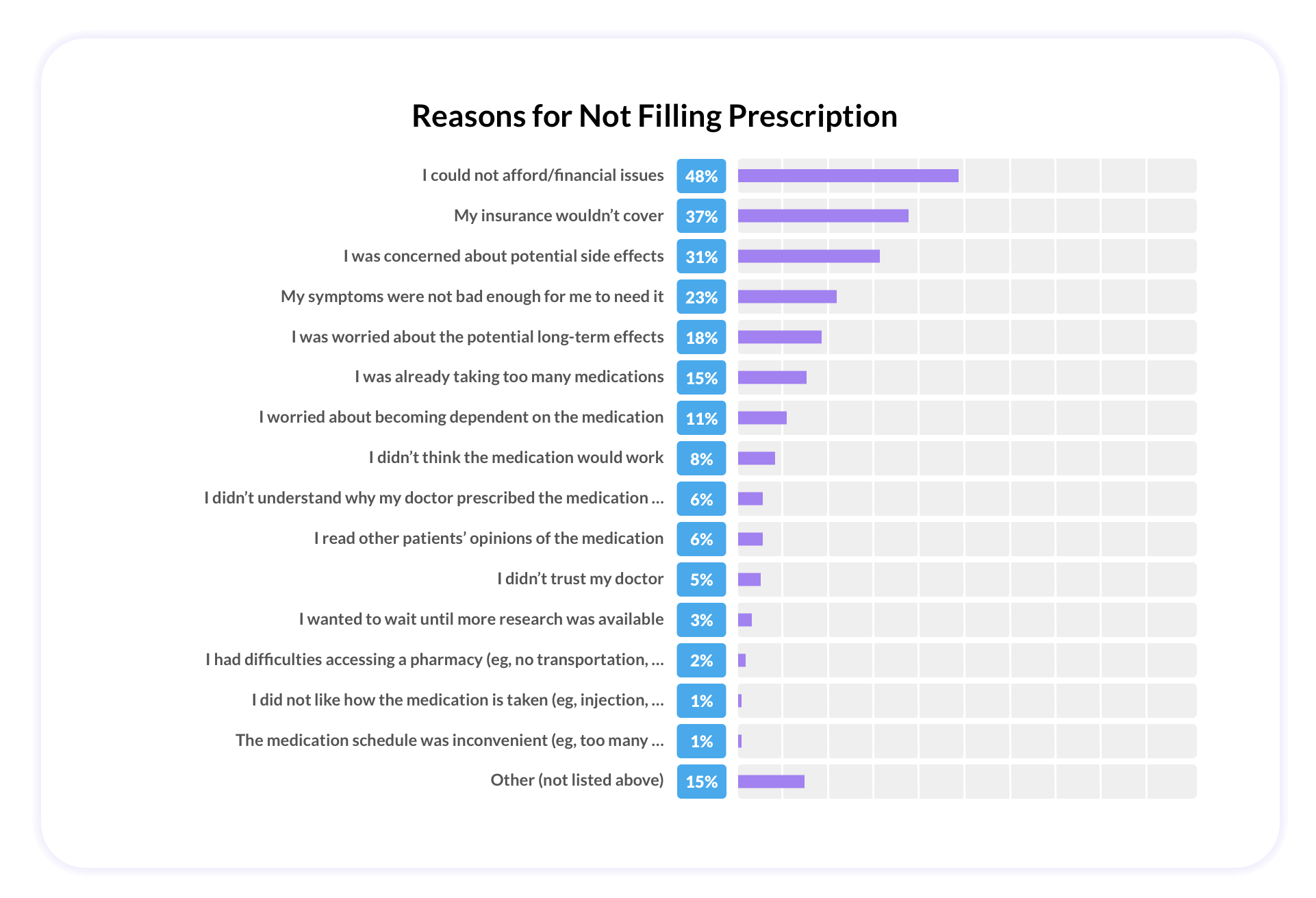
At the beginning of a patient’s prescription journey, of the quarter of patients who chose not to fill a new prescription, 57% cited that financial and/or insurance issues were the reason.
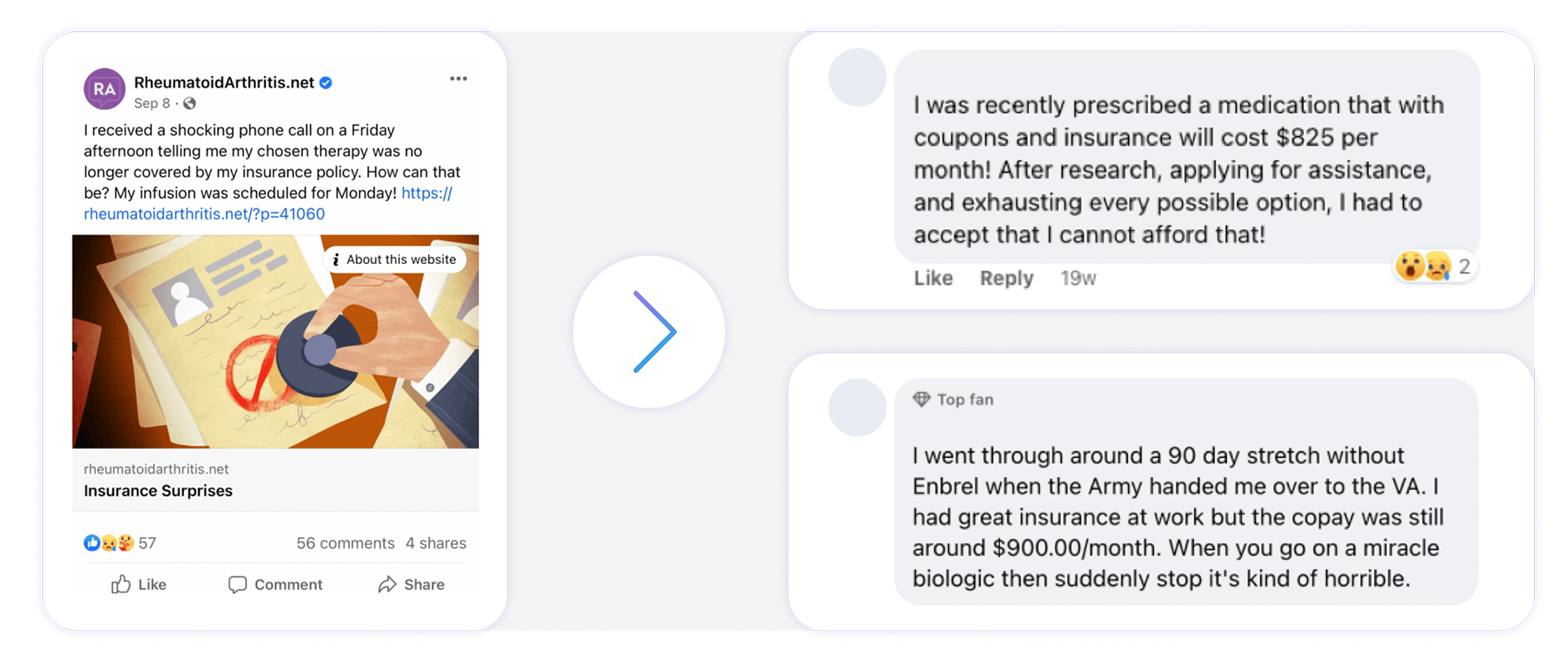
Health Union’s online community model demonstrates the everyday challenges patients face in making treatment decisions when facing difficult financial situations.
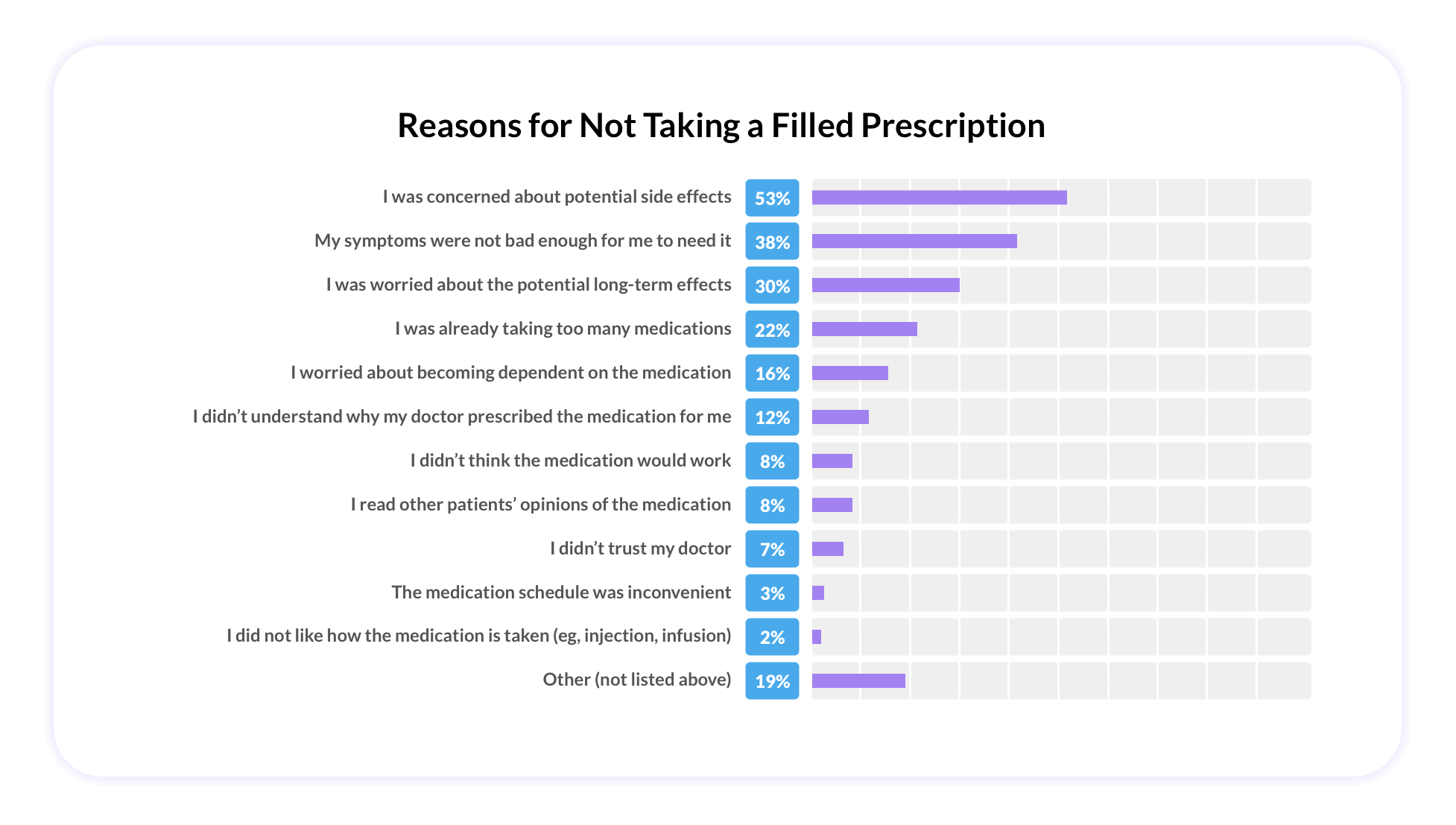
Once patients have the prescription in hand, the challenges shift from financial to behavioral and emotional. The perception and experience of side effects plays a leading role in whether patients will start and stop therapy.
In some cases, patients will choose not to start therapy due to the fear of impending side effects. Of the 12% of patients who reported filling a prescription but never taking it in this survey, 53% reported that fear of side effects is what held them back.
And as it relates to stopping a medication, 48% (of the 31% of patients that stopped taking medication) cited it was due to actually experiencing side effects.
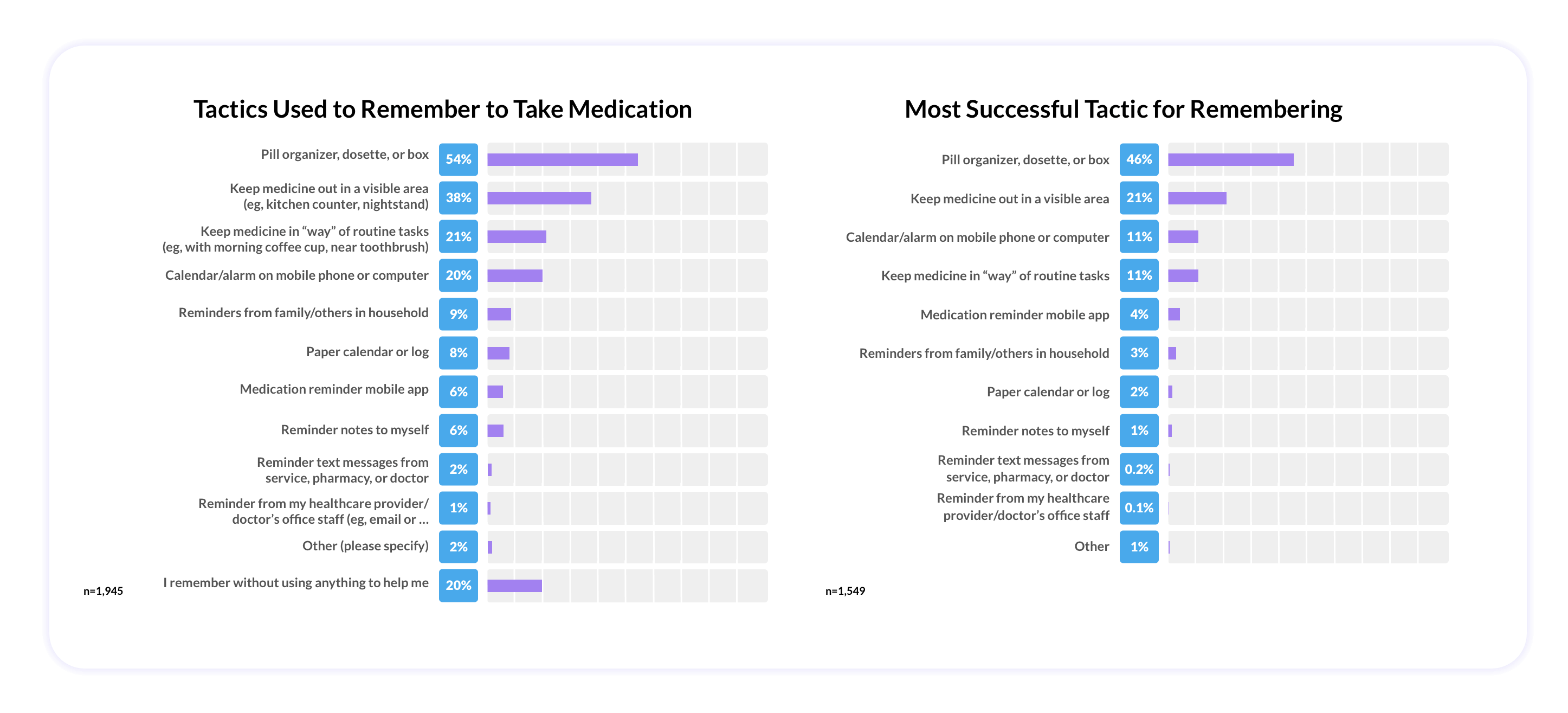
According to our data, once patients are on medications, they do their best to stay on. The charts below illustrate that 8 of 10 patients surveyed used at least one tactic to help them remember to take their medication according to schedule, many of which are reminders.
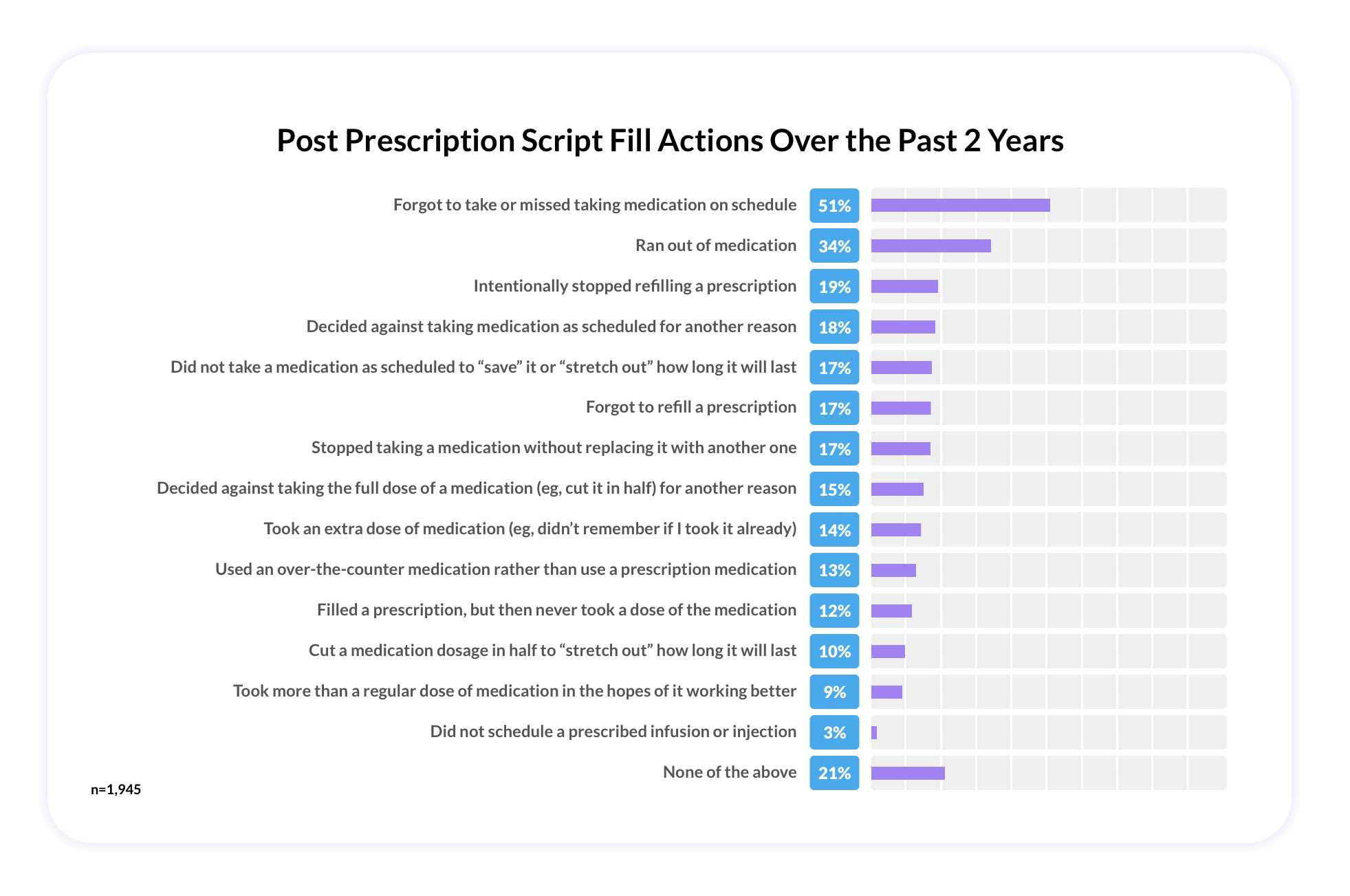
Even so, remembering to take medication is a challenge, and half of patients reported to have missed their medication on schedule in the past two years with forgetfulness topping the list (87%) as the leading reason.
Polypharmacy Presents Additional Challenges
In the United States, it’s estimated that 44% of men and 57% of women ages 65 and older are regularly using at least five medications (polypharmacy).
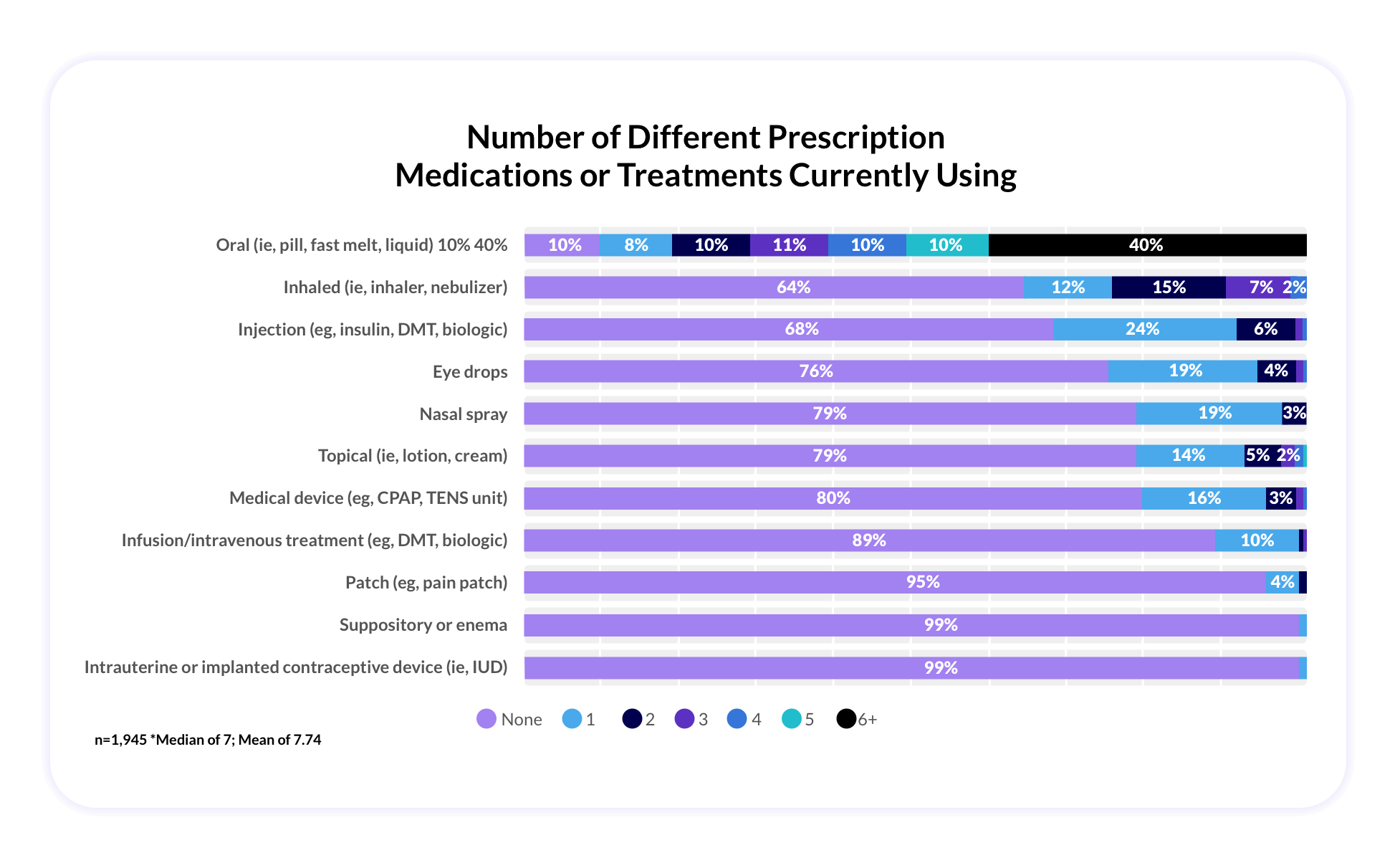
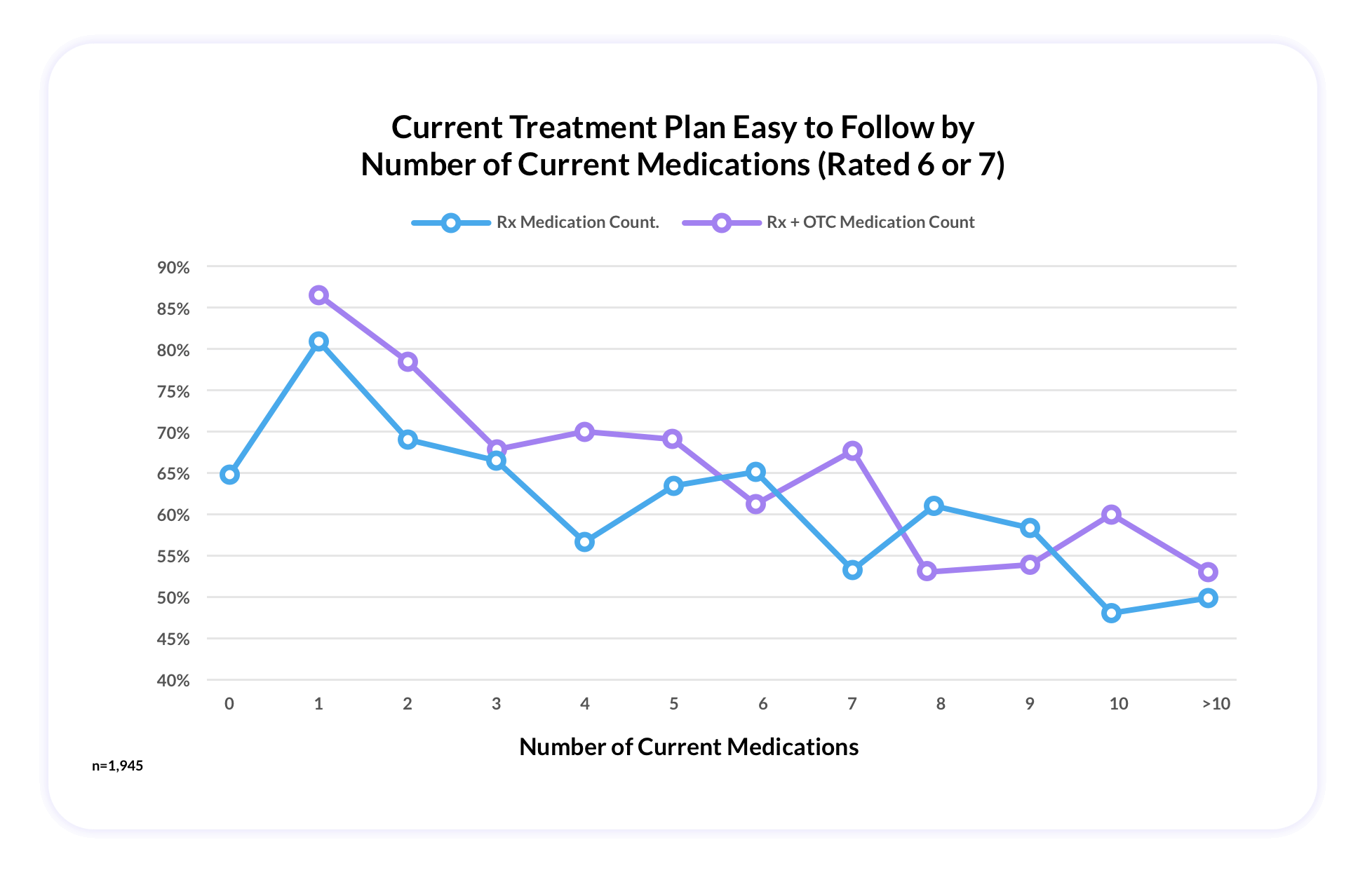
Within this survey, which included 1945 patients across 48+ different conditions, the average number of medications being used was 7 (most commonly orals), which indicates that the survey patient population was largely comprised of polypharmacy patients.
According to these patients, as the number of medications taken increases, perceived ease of following one’s treatment plan decreases, which presents an added burden.
Reaching Patients Where They Are through Social Health
The insight gleaned from this survey is that while chronic condition patients, often on a polypharmacy regimen, face substantial challenges to adherence and compliance, they are still motivated and take action to remain compliant on their treatment plans. And while conversations are still happening within the walls of the doctors office, there are real disconnects and gaps in education around adherence and compliance that must be addressed elsewhere.
Leveraging social health, the dynamic, real-time actions people take to find meaningful connections and share information throughout the health journey, as a tool to fill these gaps with the right message in the right moment at the right time, will help drive smarter, more effective health decisions.
The beauty of reaching and educating these chronic condition patients through social health, is that patients are actively engaging and seeking new solutions already through social health, the conversations are happening in real time as challenges arise.
Whether it’s advertising cost savings programs, safety profile FAQs, nurse navigator, and patient support programs, these are all topics that are already being discussed in online communities and on social media. These resources and solutions are highly relevant and shareable through social health.
Building Patient Trust through Social Health
The patient journey is not linear, nor are the challenges of adherence and compliance. However, by partnering with patients on adherence and compliance initiatives and being present within social health during the moments when people need it most, brands can show that they understand and build credibility within patient communities.
Partner with Health Union to expertly navigate the expansive world of social health – from scalable online health communities and social extensions to comprehensive quantitative condition-specific data and more.
Footnotes:
*Patients who were living with a chronic health condition who were currently using at least one medication – either prescription or OTC